Digitization of healthcare records spans decades, with the first attempts dating back to the late 1960s. As we head toward the mid-21st century, development of electronic health record systems (EHR systems) has rapidly advanced due to the emergence of a trifecta of conditions: the rise of cloud and mobile computing, the improved access and affordability of Big Data, and the wide commercialization and improvement of EHR systems.
Although strides have been made in the process of collecting – and protecting – health records for millions of patients, maintaining an EHR system is not without it’s stresses and challenges.
What follows is a comprehensive overview of health record digitization and the benefits to care providers and their patients.
Page Contents
What is an EHR System

source:neotechub.com
Put simply, it’s a system of collecting patient data and making it immediately accessible to patients, labs, and care providers regardless of location. These systems were originally created by individual hospitals, with one of the first decentralized electronic records systems being created and put to use by the Veterans Administration in the early 1970s.
Although each of the pioneering designers of EHR systems had their own protocols and delivery methods, they all had the same goal:
* Overcoming the limitations of paper records for sharing patient health and medical information
* Reducing the workload of clinical bookkeepers while maintaining accuracy
* Distilling the important information in patient records and making it widely available to clinicians, epidemiologists, managers, and patients
The rules for creating and maintaining such systems were formalized by the Edition Federal EHR Certification Rules in 2010 and 2014, and they continue to be refined and perfected today. However, the goals remain the same.
Challenges and Triumphs for Care Providers and EHR Systems
When electronic records were created by and for a handful of medical facilities, the challenge of wide-spread data sharing wasn’t so apparent. Then came the creation of disparate ambulatory centers and the need for a decentralized record collection and storage spurred by national systems like Medicare and Medicaid. These evolving conditions highlighted certain logistical issues and the need for greater supply-chain investment in software and infrastructure.
The problem was, there were more records scattered over a wider area, while storage and access were limited.
This greater need for unified standards and protocols resulted in the Health Information Technology for Economic and Clinical Health (HITECH) Act. The “meaningful use” standards adopted in the act form the backbone for creating modern EHR features that:
* Establish a set of consistent and structured clinical data that’s uniform across multiple care settings and vendor systems
* Create a system for issuing automated alerts and reminders
* Have stable, robust measurement capabilities
* Employ advanced data mining technology
* Streamline public health analysis and reporting
* Are compatible with other electronic record systems
There was initial resistance to the migration from paper to digital records due to time and cost concerns, and a fear that data breaches would lead to HIPAA violations. However, these concerns are overshadowed by the benefits of unified digital health record systems and advances in cyber-security.
It’s widely believed that 2024 will be the year that all of these elements come together to provide a comprehensive EHR system that’s less stressful and more workable for all involved. You can read more about EHR system and medical app development at yalantis.com.
Three of the biggest improvements are:
* Cloud-based services that improve records storage capacity and access
* Data analytic applications that use advanced data mining to extract and evaluate information faster and with more accuracy
* The creation of mobile medical devices that monitor patient health and transmit alerts
How EHR Systems Improve Care Delivery

source:neotechub.com
Medical outcomes are improved by making detailed, up-to-date, and accurate records available to care, providers, clinics, research facilities, and health care vendors in a timely manner. When someone’s life is potentially at risk, there’s no time for corrections and couriers to get information to the people who need it.
Since the access, affordability, and accuracy of records made available through unified EHR systems have improved, a national survey of doctors reveals that:
* 88 percent feel that their practice has benefited
* 94 percent agree that records are easier to share and access
* 75 percent feel that patient care has improved
These high rates of care provider satisfaction can be traced to the main ways that EHR systems changed the healthcare industry.
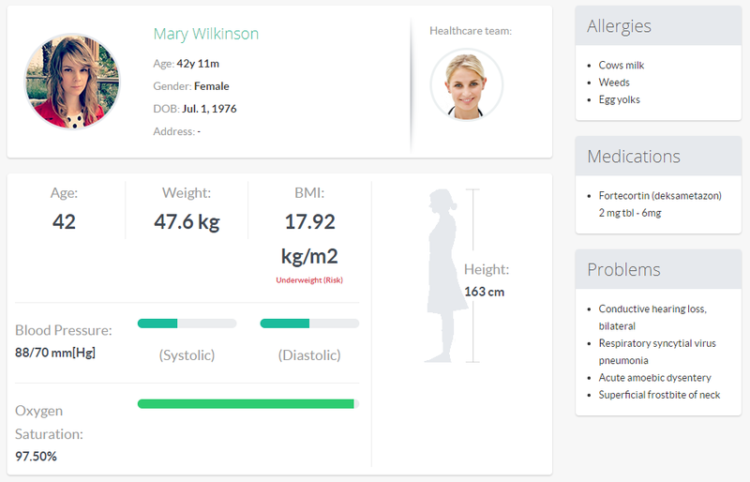
Improved Public and Private Health Outcomes
Because records are centralized and accessible, overall patient care and outcomes have increased. For example, emergency rooms will have immediate access to information about a patient’s health history, including current medications, chronic conditions, and allergies. If the patient is unresponsive, this access will save time and lives.
Electronic health records also improve public health by providing the ability to identify trends relating to a rise in certain conditions, the spread of communicable diseases, and other public health concerns.
Improved Risk Management

source:neotechub.com
Improved analysis and record accuracy also improve risk management in medical settings. Clinicians can quickly identify issues and areas of risk, and solutions can be put into place faster and more efficiently. Electronic records also provide a system of checks and balances that limits fraud. They’re also harder to steal, damage, or destroy.
Cost Reduction
Although there is an initial financial outlay for migrating from paper-based to electronic systems, the savings over time mitigate the original investment. Paper records take more time and manpower to compile and maintain. The additional storage necessary, not to mention office supplies, adds to the cost.
Cost reductions are also experienced when there are no more records to transcribe or coding errors that hold up billing. Overall documentation is also improved.
Increased Storage Capabilities

source:neotechub.com
Anyone who has ever worked in an office knows how much space is taken by physical records and files. This problem is compounded by requirements that medical records be kept on file for at least six years.
When medical records are stored on a cloud, there is an unlimited capacity to store data and make it available to anyone who needs the information. Say goodbye to office clutter and missing records.
Improved Access and Accuracy
When records are handwritten on paper, the problems of human error, illegible handwriting, and inaccurate or outdated information can lead to poor care and overlooked details that could threaten patient life and health. Electronic systems include features requiring verification, edits, and complete documentation. Because these records are stored on a cloud, they’re accessible to clinicians, doctors, and patients from any device or location.
source:ehrintelligence.com
Final Thoughts
The goal of modern EHR systems is better patient outcomes. Like medical care, technology is a constantly evolving field. The combination of advances in both are leading to a refined ability to collect and share health data that’s accurate and meaningful. This leads to improved security, greater efficiency, and conserves resources without sacrificing the quality of care.